加载中
Back pain that stops you from enjoying daily life isn’t just a minor issue—it could be a sign of lumbar disc herniation. This condition is a leading cause of lower back and leg pain in adults, especially between the ages of 30 and 50, and its impact on mobility, work, and quality of life can be profound.This article outlines common signs to watch for, possible contributing factors, and supportive approaches to daily management—such as modifying activities, using a lumbar brace, and incorporating guided exercises. Treatment options vary depending on individual needs and should be discussed with a healthcare provider.
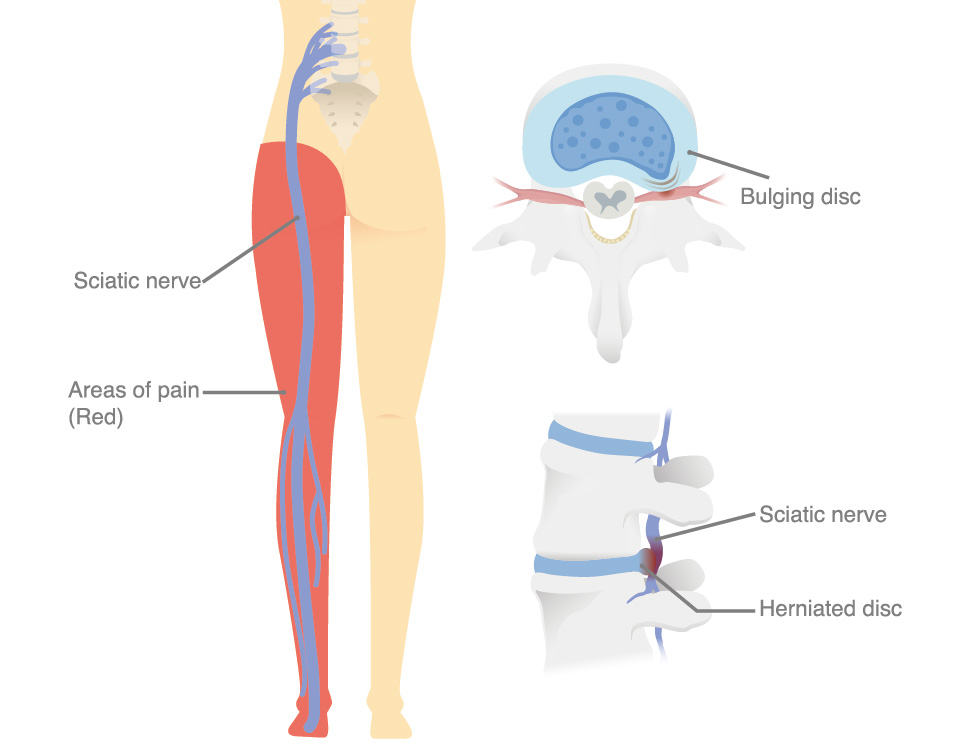
Lumbar disc herniation is a common spinal condition where the soft, gel-like center of an intervertebral disc (nucleus pulposus) protrudes through the tough outer layer (annulus fibrosus) in the lower back. This herniation can compress nearby spinal nerves, leading to back pain, leg pain (sciatica), numbness, or muscle weakness. It most frequently occurs between the L4-L5 or L5-S1 vertebrae, which bear significant weight and stress. Disc herniation may develop gradually from degenerative changes or result from sudden heavy lifting, twisting, or injury. It is one of the leading causes of lower back and leg pain in adults, particularly between the ages of 30 and 50, and can significantly impact mobility, work, and quality of life.
Symptoms vary depending on the severity and location of nerve compression but commonly include:
Lumbar disc herniation results from a combination of mechanical stress and degenerative changes in the spine. Contributing factors include:
Treatment depends on symptom severity and response to conservative care:
Can Wearing a Brace Really Help with Lumbar Disc Herniation?
Lumbar braces can be an effective part of conservative management for lumbar disc herniation, particularly during the acute phase of symptoms. Their benefits include:
Spinal stabilization: By limiting excessive forward bending, twisting, and side-bending, lumbar braces help protect the injured disc and prevent aggravation of nerve compression. This mechanical support reduces micro-movements between vertebrae, giving inflamed tissues a chance to recover.
Load distribution and unloading of the spine: Braces can help transfer part of the upper body load to the pelvis and abdomen, reducing the mechanical stress on the herniated disc.
Postural correction: Many braces promote a neutral lumbar curvature, preventing prolonged flexion or slouching that can worsen disc bulging and nerve irritation. Improved posture also reduces compensatory muscle strain in the lower back.
Pain modulation: Limiting painful ranges of motion and providing gentle compression may help reduce muscle spasms and inflammation, easing both local back pain and radiating leg pain.
Proprioceptive feedback and movement control: Wearing a brace increases awareness of body positioning, reminding patients to move more cautiously and avoid high-risk activities during recovery.
Confidence during daily activities: Patients often report feeling more secure when wearing a brace, which allows them to resume light work, walking, or gentle exercise sooner without fear of re-injury.
Copy Link