LOADING
Back pain that stops you from enjoying daily life isn’t just a minor issue—it could be a sign of lumbar disc herniation. This condition is a leading cause of lower back and leg pain in adults, especially between the ages of 30 and 50, and its impact on mobility, work, and quality of life can be profound.This article outlines common signs to watch for, possible contributing factors, and supportive approaches to daily management—such as modifying activities, using a lumbar brace, and incorporating guided exercises. Treatment options vary depending on individual needs and should be discussed with a healthcare provider.
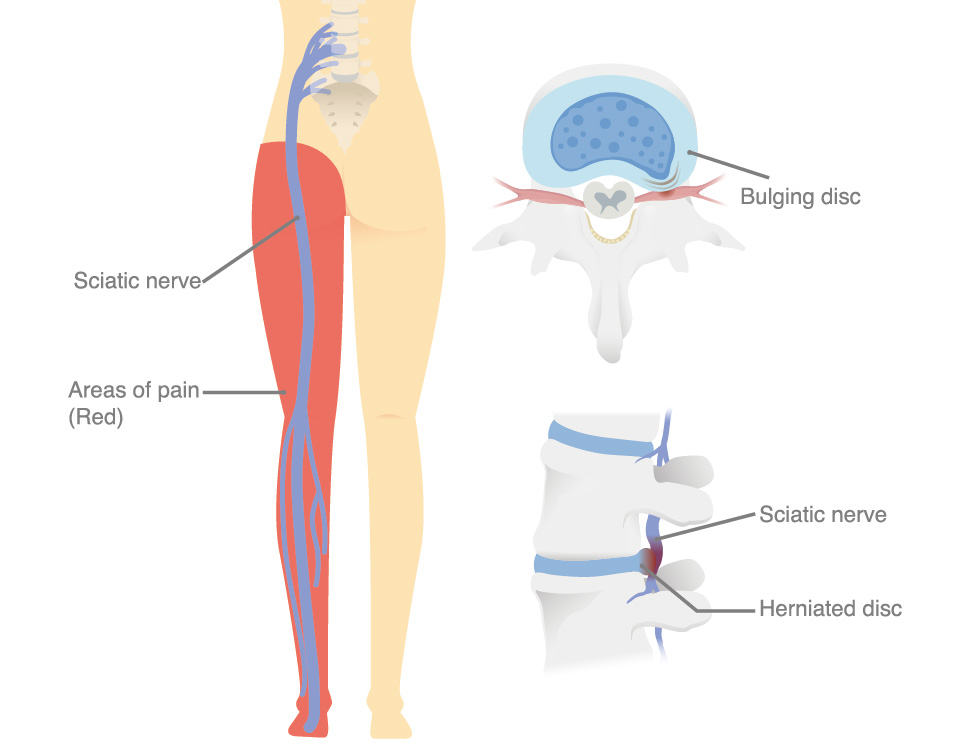
Lumbar disc herniation is a common spinal condition where the soft, gel-like center of an intervertebral disc (nucleus pulposus) protrudes through the tough outer layer (annulus fibrosus) in the lower back. This herniation can compress nearby spinal nerves, leading to back pain, leg pain (sciatica), numbness, or muscle weakness. It most frequently occurs between the L4-L5 or L5-S1 vertebrae, which bear significant weight and stress. Disc herniation may develop gradually from degenerative changes or result from sudden heavy lifting, twisting, or injury. It is one of the leading causes of lower back and leg pain in adults, particularly between the ages of 30 and 50, and can significantly impact mobility, work, and quality of life.
Symptoms vary depending on the severity and location of nerve compression but commonly include:
Lumbar disc herniation results from a combination of mechanical stress and degenerative changes in the spine. Contributing factors include:
Treatment depends on symptom severity and response to conservative care:
Rest and activity modification: Avoid heavy lifting and prolonged bending, but maintain gentle mobility to prevent stiffness.

Lumbar braces can be an effective part of conservative management for lumbar disc herniation, particularly during the acute phase of symptoms. Their benefits include:
✓ Spinal stabilization: By limiting excessive forward bending, twisting, and side-bending, lumbar braces help protect the injured disc and prevent aggravation of nerve compression. This mechanical support reduces micro-movements between vertebrae, giving inflamed tissues a chance to recover.
✓ Load distribution and unloading of the spine: Braces can help transfer part of the upper body load to the pelvis and abdomen, reducing the mechanical stress on the herniated disc.
✓ Postural correction: Many braces promote a neutral lumbar curvature, preventing prolonged flexion or slouching that can worsen disc bulging and nerve irritation. Improved posture also reduces compensatory muscle strain in the lower back.
✓ Pain modulation: Limiting painful ranges of motion and providing gentle compression may help reduce muscle spasms and inflammation, easing both local back pain and radiating leg pain.
✓ Proprioceptive feedback and movement control: Wearing a brace increases awareness of body positioning, reminding patients to move more cautiously and avoid high-risk activities during recovery.
✓ Confidence during daily activities: Patients often report feeling more secure when wearing a brace, which allows them to resume light work, walking, or gentle exercise sooner without fear of re-injury.
If you’re managing lumbar disc herniation, a supportive brace can ease discomfort and improve posture. Explore how OPPO’s Adjustable Back Support and Lumbar Dual-secure provide targeted stabilization and lasting relief.
Exercise is essential in the rehabilitation of lumbar disc herniation to improve flexibility, strengthen the core muscles, and support spinal stability. Always start with gentle movements and progress under professional supervision.
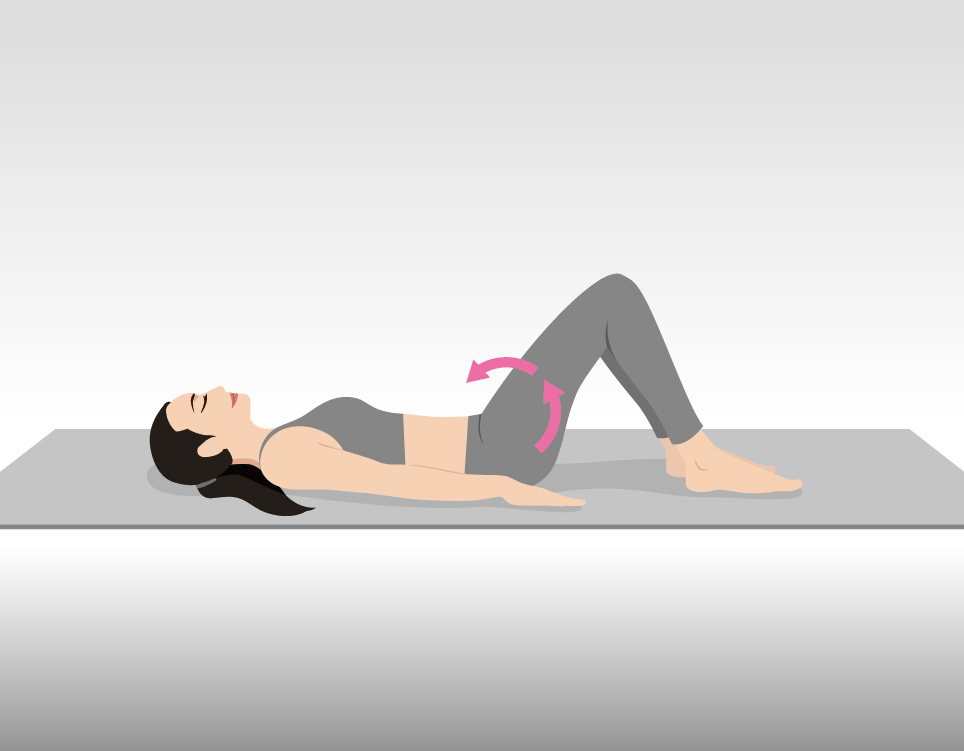
Lie on your back with knees bent and feet flat. Tighten your abdominal muscles and press your lower back gently into the floor. Hold for 5 seconds, then relax.
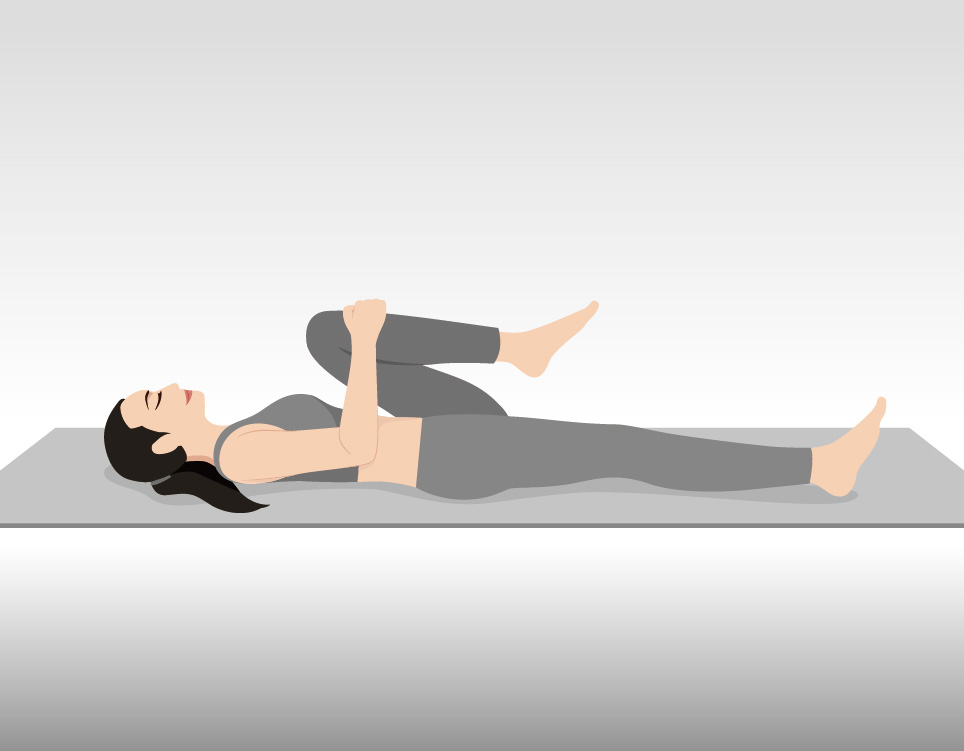
Lie on your back with knees bent. Gently pull one knee toward your chest while keeping the other foot flat on the floor. Hold for 15–30 seconds, then switch legs.
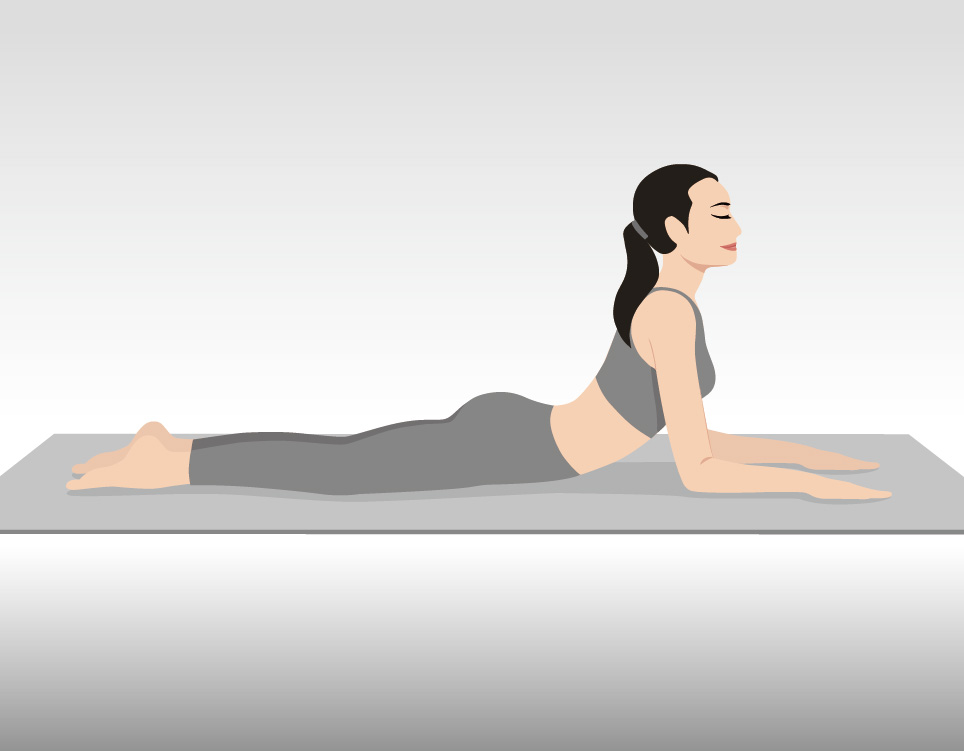
Lie face down, hands under your shoulders. Slowly press your upper body upward, keeping your hips and legs on the floor. Do not force the movement into pain. Hold for 1–2 seconds, then return.
Sit upright in a chair. Place your hands on your lower back and gently arch backward, lifting your chest. Hold for 2–3 seconds, then return to neutral.
A: Herniated lumbar discs usually get better over time, but the recovery speed can be quite different from person to person. Research shows that most people start to feel better within about four weeks (Humphreys et al., 1999). Around 60–80% of patients recover within 6 to 12 weeks, and about 80–90% see their symptoms go away in the long run, usually within a year or more (Kögl et al., 2024). That said, not everyone follows the same timeline—some people improve in just a week or two, while others may continue to have pain for months or even longer (Benoist, 2002).
A: Most people with a herniated disc can live a normal, active life if they manage it properly through physical therapy, exercise, healthy habits, and medical care when needed. Research shows that individuals with herniated discs can often maintain functional lives, being able to work or engage in regular sports activities. (S. Weber et al., 1985). With proper care, even with occasional flare-ups or chronic pain, people can maintain function, independence, and a full, productive life.
A: Yes! Many herniated discs can heal and improve without the need for surgery. Research shows that your body has a remarkable ability to heal itself. In many cases, a herniated disc can shrink and resolve on its own through a process called resorption. Studies indicate that most cases of lower back pain caused by a herniated disc get better without surgery, though symptom duration can vary from weeks to months (Benoist, 2002). In fact, many patients respond well to conservative treatments like physical therapy, which can significantly reduce the need for an operation (Ito et al., 2001).
A: Walking is a low-impact activity that is generally beneficial for people with a herniated disc. It improves blood flow to the spine, supporting healing and reducing inflammation, while gently strengthening the core, lower back, and hip muscles to lessen strain on the affected disc. Research also shows that walking, especially after surgery, can reduce pain, decrease disability, and improve quality of life(Aldemir & Gürkan, 2021; Uysal et al., 2023). Start with short walks and gradually increase as tolerated, always maintaining good posture and walking on even, soft surfaces. Stop if pain, numbness, or weakness occurs, and consult a doctor if symptoms worsen.
A: When we talk about the stages of a herniated disc, doctors typically classify into four distinct stages (Malarvizhi & Balamurugan, 2022):
1. Degeneration: The disc begins to wear down, often due to age.
2. Prolapse: The disc bulges outward, but its outer layer is still intact.
3. Extrusion: The outer layer of the disc tears, and the soft, inner material squeezes out.
4. Sequestration: A piece of the inner material breaks off completely and can move freely.
Copy Link